Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that affects the large intestine (colon) and rectum. This essay aims to shed light on the complexities of UC, including its definition, causes, symptoms, diagnostic methods, treatment options, and the impact it has on individuals’ lives. Understanding this condition is crucial for managing symptoms, improving quality of life, and fostering a supportive environment for individuals with UC.
Defining Ulcerative Colitis:
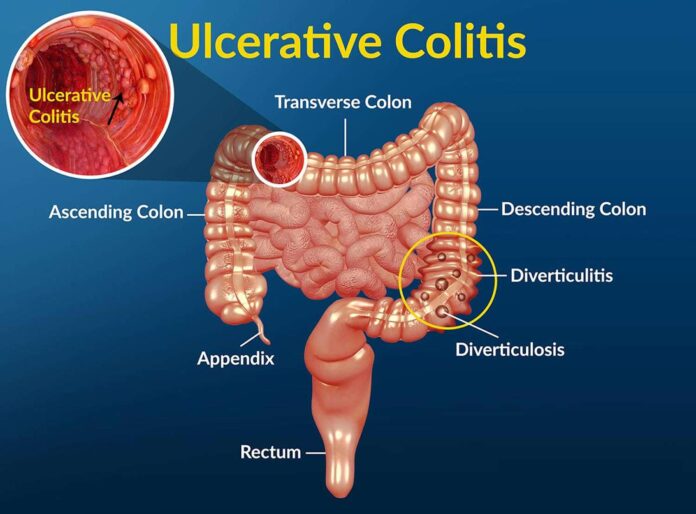
Ulcerative colitis is an autoimmune disease characterized by chronic inflammation of the colon and rectum. It is a form of inflammatory bowel disease (IBD) alongside Crohn’s disease, and it primarily affects the innermost lining of the colon. The inflammation leads to the formation of ulcers, causing symptoms such as abdominal pain, diarrhea, rectal bleeding, and urgency to have bowel movements.
Causes and Risk Factors:
The exact cause of ulcerative colitis remains unknown, but it is believed to result from a combination of genetic, environmental, and immune system factors. A family history of UC or other autoimmune conditions increases the risk of developing the disease. Environmental triggers, such as stress, certain medications, diet, and gut microbiota, can also contribute to flare-ups and symptom severity.
Symptoms and Complications:
Ulcerative colitis presents a range of symptoms that can vary in intensity and duration. Common symptoms include diarrhea (often with blood), abdominal pain and cramping, urgency to have bowel movements, rectal bleeding, fatigue, weight loss, and reduced appetite. In severe cases, complications like bowel perforation, severe bleeding, toxic megacolon (a potentially life-threatening condition), and an increased risk of colon cancer may arise.
Diagnosis and Disease Monitoring:
Diagnosing ulcerative colitis requires a combination of medical history assessment, physical examinations, laboratory tests, and imaging studies. Colonoscopy with biopsies remains the gold standard for diagnosis, allowing direct visualization of the colon and rectum and the collection of tissue samples for microscopic examination. Additional tests, such as blood tests, stool tests, and imaging techniques like CT scans or MRI, may be used to evaluate disease severity, monitor inflammation, and rule out other conditions.
Treatment Options:
The management of ulcerative colitis aims to control symptoms, induce and maintain remission, and minimize complications. Treatment approaches vary depending on disease severity and individual factors. Medications, such as aminosalicylates, corticosteroids, immunomodulators, and biologic therapies, are commonly prescribed to reduce inflammation, modulate the immune system, and alleviate symptoms. Lifestyle modifications, including dietary adjustments, stress management techniques, regular exercise, and adequate hydration, can complement medical interventions and promote overall well-being.
Surgery and Alternative Therapies:
In cases of severe or unresponsive ulcerative colitis, surgery may be necessary. Surgical options range from removing the colon and rectum (proctocolectomy) with the creation of an ileostomy or an ileo-anal pouch procedure. Surgery can provide long-term relief from symptoms and improve quality of life. Alternative therapies, such as probiotics, herbal remedies, and mind-body techniques like acupuncture and yoga, may be explored as complementary approaches, but their efficacy and safety should be discussed with healthcare professionals.
Impact on Quality of Life:
Ulcerative colitis significantly impacts individuals’ lives, both physically and emotionally. The chronic nature of the disease, frequent symptom flares, and potential complications can cause disruptions in daily activities, work productivity, social interactions, and mental well-being. Coping with the challenges of a chronic illness, managing treatment regimens, and navigating the emotional toll requires a comprehensive approach that addresses not only the physical aspects but also the psychological and social dimensions of living with UC.
Support and Self-Care:
Creating a supportive environment for individuals with ulcerative colitis is essential for fostering well-being and reducing the stigma associated with the condition. Education and awareness initiatives can promote understanding among family, friends, colleagues, and the general public. Support groups, counseling, and patient advocacy organizations provide opportunities for individuals to connect, share experiences, and access valuable information. Self-care practices, such as stress management techniques, maintaining a balanced diet, prioritizing rest and relaxation, and regular medical follow-ups, empower individuals to actively manage their condition and improve their quality of life.
Ulcerative colitis is a chronic inflammatory bowel disease that poses significant challenges for individuals living with the condition. By understanding the disease’s definition, causes, symptoms, diagnostic methods, treatment options, and impact on quality of life, we can foster a supportive and informed environment. With comprehensive medical care, effective treatments, and self-care practices, individuals with UC can manage symptoms, achieve remission, and lead fulfilling lives. Continued research, advocacy, and awareness efforts are essential in improving the understanding, treatment, and overall well-being of individuals affected by ulcerative colitis.